A trial of a multilevel upper airway surgery has led Australian experts to promote it as an option to specialists around the world for managing difficult obstructive sleep apnea (OSA) cases.
A new study of the surgery shows efficacious outcomes in sleep apnea patients who had been unable to use CPAP treatment, with patients achieving relief from snoring and disrupted sleep and experiencing improved general health, according to a new report in the Journal of the American Medical Association (JAMA).
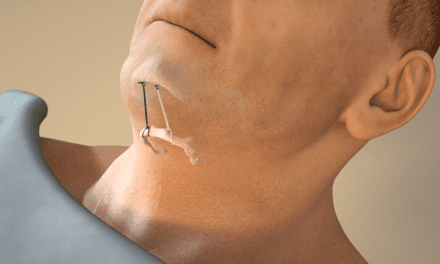
The multi-level surgical technique combining a new version of palate surgery with a tongue procedure to create an improved airway resulted in a substantial reduction in the number of night-time apnea events and improvements in daytime sleepiness and quality of life. After removing any tonsils, the palate is repositioned and the tongue treated to open up the airway and reduce obstruction.
Study findings include:
- The trial participants were recruited from six clinical centers in three Australian states (SA, NSW, and WA) and were predominantly overweight males with severe OSA who could not satisfactorily use standard medical treatments.
- Of the 102 people in the trial, 51 were randomly assigned to receive the OSA surgery, the other 51 to continue with best possible medical treatment.
- After six months, those receiving the surgery had an approximate 60% decrease in the frequency of throat obstructions at night compared with a 20% decrease in participants who remained on medical treatment, and had major added improvements in snoring, daytime sleepiness, and general health status.
- A total of seven surgeons performed the multilevel surgery across the six clinical centers using techniques pioneered in Australia by the late ear-nose-throat (ENT) physician Sam Robinson and subsequently refined and standardized for the trial by professors Stuart MacKay, Bsc (Med), MBBS (Hons), FRACS, and Simon Carney, MD.
- The trial was the brainchild of the late Nick Antic, MBBS, FRACP, PhD, a Flinders University professor and SA Health respiratory and sleep specialist, who led the study until his death in 2016.
Flinders University’s Emeritus Professor Doug McEvoy, MD, FRACP, says the surgery offers promise to millions of people around the world who have OSA but can’t adapt to using a CPAP mask or similar device each night.
“This trial is the result of extensive prior research into the surgical treatment of sleep apnea and gives new hope to people who, without treatment, would each day continue to feel sleepy and depressed and may have their lives cut short by the detrimental effects of long-term interrupted sleep,” says McEvoy in a release.
Lead author University of Wollongong professor Stuart MacKay, MBBS (Hons), FRACS, who will give further details of the surgical clinical trial at the global online European Respiratory Society congress on 7 September and in a JAMA podcast, says about half of patients prescribed CPAP treatment are not using it consistently long term. “It’s very exciting to see so many patients getting a better night’s sleep with reduced snoring and less health risk after this surgery, ” says MacKay in a release.
Surgery animation: After removing any tonsils, the palate is repositioned and the tongue treated to open up the airway and reduce obstruction. Credit: Simon Carney, professor and ENT surgeon
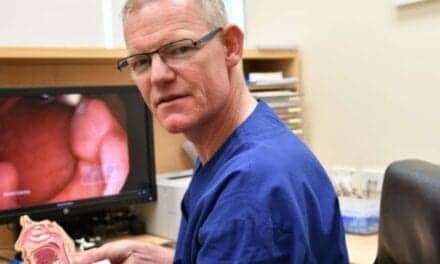
Photo: Flinders University professor Doug McEvoy, who worked with ENT surgeons including Stuart MacKay on refining the new procedure. Credit: Flinders Foundation