11/03/06
Preliminary research suggests that brainstem abnormalities involving certain serotonin pathways in the brain may play a more important role in SIDS than previously thought, according to an article in the November 1 issue of JAMA.
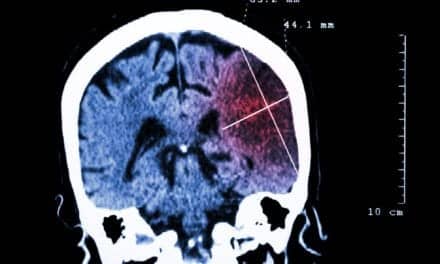
SIDS is the leading cause of postneonatal infant death in the United States. Despite intensive research, the causes of SIDS remain unknown, according to background information in the article. Previous research has suggested that abnormalities in the receptor (a structure on the surface or inside a cell) binding of the serotonergic (5-hydroxytryptamine [5-HT]) neurons in the medulla (the section of the brainstem that regulates breathing) may play a role in SIDS.
David S. Paterson, PhD, of Children’s Hospital Boston and Harvard Medical School, Boston, and colleagues examined the relationship between SIDS cases and cellular defects associated with altered 5-HT receptor binding in the 5-HT pathways in the medulla of the brain. The researchers analyzed frozen samples of the medulla from 31 infants who died from SIDS (cases) and from 10 infants who died from causes other than SIDS (controls). The brain tissues were obtained from the San Diego Medical Examiner’s office between 1997 and 2005. Markers of 5-HT function were compared between SIDS cases and controls. The number of samples available for each analysis ranged from 16 to 31 for SIDS cases and 6 to 10 for controls. An exploratory analysis of the correlation between markers of HT function and 6 recognized risk factors for SIDS also was performed.
"We found that the medullary 5-HT abnormalities in SIDS are more extensive than previously suggested and that they involve multiple elements of 5-HT function, including 5-HT neuron count, 5-HT1A receptor expression, and relative 5-HT transporter binding in the same cases. This study strengthens the hypothesis that medullary 5-HT dysfunction is associated with SIDS and may lead to death by a failure of respiratory and autonomic responses [functions of the nervous system not under voluntary control, e.g. the regulation of heartbeat or gland secretions] to homeostatic [internal regulatory] stressors during sleep," the authors write.
"This study also found, in an explanatory analysis, reduced 5-HT1A receptor binding density in male compared with female SIDS cases, an observation that may help explain why males are more vulnerable to SIDS. These 5-HT abnormalities were documented during the era of stringent public messages on risk reduction, including that for supine sleep position. The majority (65%) of the SIDS cases in this data set, however, were sleeping prone or on their side at the time of death, indicating the need for continued public health messages on safe sleeping practices."
The researchers speculate that the increased risk of SIDS in the prone or face-down position may reflect the infants’ inability to respond to the challenge to breathe in the face-down position, due to the abnormalities in the medullary 5-HT system that compromise protective reflexes, including arousal and head turning.
"This study provides biological plausibility for certain risk reduction strategies in SIDS …," the authors write. "Moreover, it generates new hypotheses for testing about 5-HT-related brainstem pathology underlying sudden death in early life in future SIDS autopsies and in experimental mechanistic models."