Survey: Due to COVID-19, Sleep Medicine Professionals Turn to Telemedicine, Mail-Order Services to Manage Patients; Some Facilities Close, While Others Remain Mostly Business-as-Usual (Survey Closed April 10)
By Sree Roy
Sleep Review initiated an informal online-only survey to gather and share data on novel coronavirus SARS-CoV-2 pandemic-related impacts to sleep medicine practices and sleep disorders centers. The Google Forms survey started on March 17 and concluded on April 10 (n=306) and was available to sleep medicine professionals via www.sleepreviewmag.com/practice-management/coronavirus-impact-sleep-medicine, where the preliminary and final results are now housed.
As with any survey, the results of this one come with several important caveats, which include that survey-takers were only those who were readers of SR online offerings and/or exposed to our social media channels.
Although this report does not capture the responses per day, I included a couple of examples of how the answers changed during the 24-day survey; business conditions worsened appreciably even over the course of the survey, particularly as government agencies and professional organizations recommended the closure of “non-essential” businesses.
Is sleep medicine essential? “Sleep care is essential to health, but the timing and delivery of this care need to be specific to each patient,” president of the American Academy of Sleep Medicine (AASM) Kelly Carden, MD, MBA, told us in an interview for an online article on that topic, adding that “There is no substitute for the medical judgment of a sleep clinician.”1 The AASM has since updated its COVID-19 Mitigation Strategies for Sleep Clinics and Labs advisory to recommend that in-lab polysomnography studies and in-lab administration of CPAP should be postponed “except in emergencies,” though the recommendations leave what qualifies as an emergency up to each clinician.2
Because various cities and regions of the United States and Canada (and the world) have been impacted differently by COVID-19—and the following statistics do not account for geography—this survey should be looked at only as a general snapshot of how the public health emergency is affecting the subspecialty. Hopefully, it will add some context to your own situation and allow sleep professionals and industry experts to better appreciate this dynamic and quickly evolving situation.
In-Facility Patients
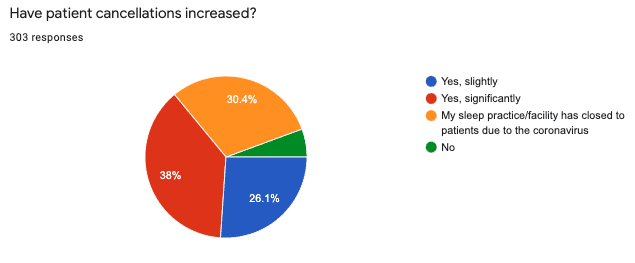
All but a small minority (5.6%) of sleep medicine facilities experienced an increase in patient cancellations. Thirty-eight percent of survey respondents reported a significant increase in patient-initiated cancellations and 26.1% reported a slight increase. The latest response that indicated no increase in cancellations was received on March 20, and the latest response that indicated only a slight increase was received on April 4.
Just under a third (30.4%) of respondents indicated that their facilities had closed to patients. Most sleep medicine professionals who work in facilities that had closed to patients could not forecast when the facility would reopen. In some cases, administration indicated a reevaluation date of 2 to 6 weeks from the time of closure. In other cases, no reevaluation or reopen date was discussed with staff.
Sleep Care Delivery
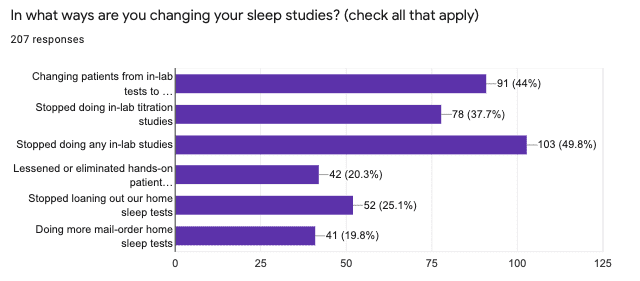
Half of respondents (49.8%) reported that their facilities stopped all in-lab sleep studies during the pandemic. But, for patients who remained willing to come in, some centers remained mostly business-as-usual, including conducting CPAP titration studies—despite evidence that noninvasive ventilation can aerosolize the virus and thereby increase the risk of spreading it to anyone physically nearby.3 Anecdotally, some sleep disorders center workers fear for their health but have a greater fear of job loss or other retribution if they refuse to participate in in-lab studies or other risky tasks. For emergency or unavoidable in-person visits, the AASM advises that workers utilize personal protective equipment (PPE).2
In some cases, sleep providers have moved care delivery to patients’ homes, without an in-facility visit. Just under half (44%) report that they are changing patients from in-lab tests to home sleep tests (HSTs), when possible. But a quarter of respondents (25.1%) say their facilities have stopped loaning out their own HST devices, presumably because of in-person touchpoints and/or cleaning and disinfection concerns. And a fifth of respondents (20.3%) have lessened or eliminated hands-on patient education before HST use. A fifth of respondents (19.8%) report an increase in the number of mail-order HSTs, which typically remove all direct in-person touchpoints.
The AASM recommends disposable home sleep tests and advises that reusable devices be removed from service for at least 72 hours in addition to disinfection before the next use, which anecdotally at least some labs are incorporating. The AASM also states that patients should not have to leave their home to receive or return the device,2 but anecdotally, some facilities are doing curbside or other non-home-based pickups/dropoffs. Video (versus live in-person) patient instruction is being incorporated more often for home sleep testing device use.
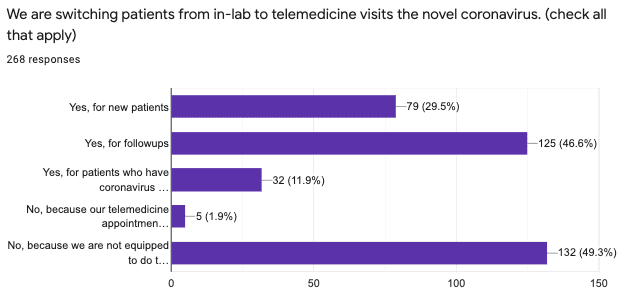
Even prior to COVID-19, telemedicine has been growing, albeit slowly, in sleep medicine. Those facilities that were equipped for telemedicine have an advantage during the pandemic, as they are able to see patients virtually. Just under half of respondents (46.6%) switched patients from in-person visits to virtual visits for followups. Just under a third (29.5%) switched new patients to virtual visits.
But half of respondents (49.3%) cannot switch patients to virtual visits because they are not equipped to do so.
In some cases, sleep practices that were equipped to do telemedicine encountered new obstacles due to server capacity (as there is a surge in virtual visits nationwide). In some cases, telemedicine companies that offered free introductory services suspended those due to lack of bandwidth.
Acting under emergency authority, the US Department of Health and Human Services (HHS) has waived most of the roadblocks for seamless Medicare coverage and delivery of telehealth services during the pandemic. For example, Medicare will cover telehealth encounters with patients wherever they are located—whether urban, rural, suburban, in health care facilities, or even from the patient’s own home. During the emergency, the HHS Office for Civil Rights will waive Health Insurance Portability and Accountability Act violation penalties for health care providers who serve patients in good faith through common laptop or smartphone programs such as Skype or Apple FaceTime.4
Work Schedule Changes
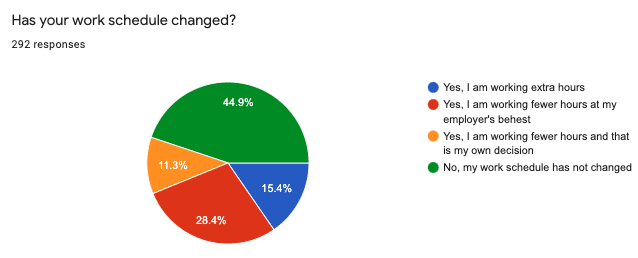
Just under half of respondents (44.9%) report that their work schedule has not changed. This response remained frequent even during the latter days of the survey. This may be due to administration who must continue to be available, perhaps in a virtual capacity, to patients and staff. Also this may represent workers who must continue to respond to patient phone and email inquiries, as well as to score and interpret home sleep tests. (The survey did not ask for job titles.)
Forty percent reported working fewer hours. Of those, 28.4% worked less at their employer’s behest and 11.3% at their own discretion. Fifteen percent reported working extra hours, likely due to being reallocated to a department in need of extra personnel due to COVID-19. For example, respiratory therapists who work in hospital-based sleep labs may be transferred to the intensive care unit to manage ventilator settings. Anecdotally, some accept these reassignments only begrudgingly.
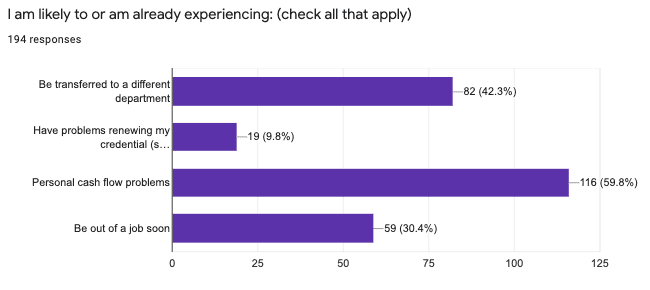
Indeed, in a separate question, 42.3% of respondents report they are likely to be or are already transferred to a different department. Unfortunately, more than half (59.8%) of sleep medicine professionals reported that they anticipate having personal cash flow problems and 30.4% think they will be “out of a job soon.” Anecdotally, sleep professionals, particularly sleep technologists, are being laid off or furloughed, and are getting by on unemployment benefits and hope that they will be back at work when the pandemic is under control. Cash flow problems were echoed at the highest levels of our survey, as many respondents indicated in an open-ended question that their major concerns surrounded how to retain staff until their sleep business returns to more typical patient numbers and delivery methods.
Cleaning and Disinfection
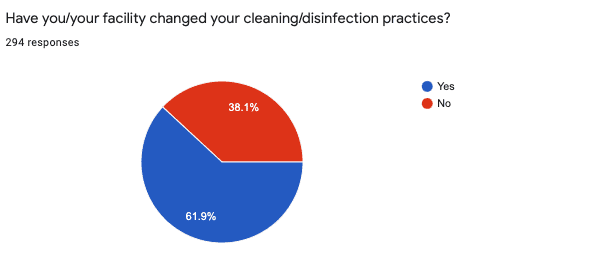
Sixty-two percent of respondents reported that facility cleaning and disinfection practices changed, while the remaining 38% report these practices stayed the same as prior to COVID-19. The most common response to an open-ended question about ways cleaning/disinfection changed was increased frequency of surface cleaning, particularly of high-touch areas such as doorknobs and lamp switches. Other common responses included increased handwashing and hand sanitizer use for staff and patients, switching to stronger cleaners/disinfectants, and using more disposable equipment and accessories.
Several respondents said their facility had instituted patient pre-screenings, with some reporting on-site temperature checks (patients with fevers were either sent home or referred to a physician for diagnosis of fever-related symptoms). A few reported that reading material was removed from patient areas; that workers were donning PPE, such as masks and gloves; that patients were allowed to wait only in private rooms (not in shared waiting rooms); that their facilities were rotating the use of specific patient rooms; and that they were intaking only one patient at a time. One respondent indicated that their facility was keeping all inside doors open to prevent patients from touching handles.
In response to a multiple-choice question about what items sleep professionals were trying to buy, the most common response was PPE (71.5%) and the second was surface cleaners/disinfectants (70.1%). (Survey-takers could select more than one response.) But PPE (including N95 masks) and cleaners/disinfectants (including hand sanitizer and disinfecting wipes) were also the items that many were unable to procure, due to nationwide shortages, according to a separate open-ended question. A few reported trouble buying thermometers.
Needed Equipment, Devices, and Services
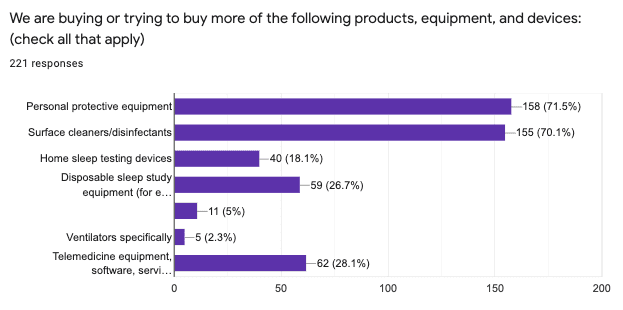
The most common sleep medicine-specific response to the multiple-choice question about what professionals were trying to buy was telemedicine medicine equipment/software/services (28.1%), with some responding in the open-ended question that they were having trouble getting telemedicine services set up.
Just over a quarter of respondents (26.7%) reported buying more disposable sleep study equipment (such as disposable electrodes) and 18.1% reported buying more HST devices.
Sleep Review thanks those sleep medicine professionals who took the time to complete this survey and share their information with their colleagues.
Sree Roy is editor of Sleep Review.
References
- Thompson G. Is sleep medicine “essential”? Sleep Review. 3 Apr 2020: https://sleepreviewmag.com/practice-management/sleep-medicine-essential-covid19.
- American Academy of Sleep Medicine. COVID-19 mitigation strategies for sleep clinics and labs – updated. 8 Apr 2020: https://aasm.org/covid-19-resources/covid-19-mitigation-strategies-sleep-clinics-labs.
- Hawryluk M. Not so fast using CPAPs in place of ventilators. They could spread the coronavirus. Kaiser Health News. 27 Mar 2020: https://khn.org/news/covid19-ventilator-shortage-substituting-cpaps-could-spread-coronavirus.
- Brown DB. Telemedicine legal update 2020. Sleep Review. 30 Mar 2020: https://sleepreviewmag.com/practice-management/laws-regulations/telemedicine-legal-update-2020.
Survey: Due to COVID-19, In-Lab Sleep Studies Being Replaced by Home Studies or Postponed Indefinitely (as of 3/24/20 at 9:00 am)
By Sree Roy
To limit the spread of the coronavirus to sleep disorders center workers and to patients, as well as to conserve personal protective equipment for emergencies, just under half of facilities (45%) report that they have stopped doing any in-lab studies, according to Sleep Review survey results (n=259). Forty-five percent also report changing at least some patients from in-lab polysomnography to home sleep testing. Thirty-six percent say they have stopped doing in-lab titration studies specifically, 21% have stopped loaning out their home sleep testing (HST) devices, 20% are doing more mail-order home sleep tests, and 20% have lessened or eliminated hands-on patient education about how to use a HSTs. (Respondents could check all that applied, so results add up to more than 100%.)
Unfortunately, these changes mean that sleep professionals are increasing finding themselves without income. More than 50% report that they are likely to or are already experiencing personal cash flow problems (57.8%) and over a quarter say they will likely be out of a job soon (27.7%); about 1 in 10 reports that they will have problems renewing their credential due to the cancellation of in-person conferences (9.6%). But 42.2% expect or already have been transferred to a different department at their healthcare facility.
Survey: Sleep Medicine Facilities Have Trouble Procuring Personal Protective Equipment, Telemedicine Services (as of 3/19/20 at 11:45 pm)
By Sree Roy
Like many other healthcare facilities during the coronavirus pandemic, sleep medicine facilities report needing to buy more personal protective equipment (PPE) but are having trouble finding it available for purchase due to high demand.
Sleep Review survey results (n=205) show that 68.2% of sleep professionals report buying or trying to buy more PPE. But in a response to a followup question that asks what products, equipment, or services they have been unable to procure so far, many responses are similar, with respondents indicating that items such as “masks,” “N95 masks,” “PPE,” “masks and alcohol gel” have been challenging or impossible to obtain. Consumer news outlets such as CNN report that some healthcare facilities have resorted to making their own personal protective equipment, as the government works to increase production of needed supplies.
Another area where some sleep medicine facilities are finding themselves without needed resources is the area of telemedicine. About 30% of respondents indicate they are trying to buy telemedicine equipment, software, and/or services; however, “telemedicine” was a common response to the open-ended survey question about what sleep professionals are having trouble procuring.
In a separate survey question, half of survey respondents (50.8%) say their facilities are not equipped to do telemedicine patient appointments. The facilities that have the capability are rapidly switching patients to telemedicine visits: 45.8% of respondents say followup appointments are being switched from in-person to telemedicine; 26.6% say new patients are being seen via telemedicine, 14.1% say that patients who show symptoms of coronavirus are being switched to virtual appointments, and less than 1% say that they are not switching patients to telemedicine because their telemedicine appointments are already full. (Respondents could check all that applied, so results add up to more than 100%.)
Survey: Most Sleep Medicine Facilities Remain Open, with Increased Precautions (as of 3/18/20 at 12:15 am PT)
By Sree Roy
About two-thirds of sleep medicine facilities (including sleep disorders centers and private sleep medicine practices) remain open, though sleep professionals anticipate more of them closing by the end of March, according to preliminary results of a Sleep Review online survey (n=15) about the coronavirus pandemic. Of the about one-third of respondents who indicate that their facilities have already closed, most are not sure when they will be able to reopen their doors to patients.
Sixty percent of sleep professionals report that their facilities have changed their cleaning/disinfection practices in response to the crisis, such as disinfecting surfaces on an increased and more regimented schedule as well as having workers don personal protective equipment such as masks and gloves. Unfortunately, some respondents indicate that they are having trouble procuring personal protective equipment due to high demand.
Sleep professionals report buying (or at least trying to buy) the following in increased amounts:
- Personal protective equipment (81.8%)
- Surface cleaners/disinfectants (72.7%)
- Disposable sleep study equipment, such as disposable electrodes (45.5%)
- Telemedicine equipment/software/services (36.4%)
- Home sleep testing devices (18.2%)
- Sleep therapy devices, such as CPAPs (18.2%)
- Ventilators specifically (9.1%)
Just under 50% of respondents say their work schedules have not changed. 20% are working fewer hours at their employer’s behest; 20% are working fewer hours electively; and 13.3% are working extra hours during the pandemic.
About 13% of respondents are not experiencing patient cancellations above their norms. About a third say patients cancellations are slightly up and about a third say cancellations are up significantly.
——-
Sleep Review is gathering and sharing data on pandemic-related impacts to sleep medicine practices and sleep disorders centers. We would appreciate it you—sleep specialists, sleep disorders centers managers, sleep technologists, dental sleep medicine practitioners, and others—take the short survey below. Bookmark this page, as we will update it as survey results become available.
This survey is now closed. But Sleep Review is partnering with Needham & Company on our semi-annual survey, which includes questions about COVID-19 impacts. Needham will give you a copy of its resulting report if you take its state-of-the-industry survey: https://www.surveymonkey.com/r/QYY7RBG.




I would like to know what labs are doing in terms of disinfecting patient interfaces, tubings, filtration being used during PAP titration? Recommended solutions, etc?
CPAP tubing and humidifier chamber is cleaned by Central Sterile. We recently switched to disposable EEG leads, Thermocouple , pulse ox and RIPbelts. CPAP masks have been single patient use and sent it home with patient.
It has affected me by not getting.my meds! Mr. Dr. Quit Dec 28th! I have not been able to get another Dr. 15 years on this medication and going without is killing me! What can I do? Not wanting to go to Dr, but desperate.