With the integration of HSAT into clinical practice, applying the precise billing and coding is a critical—but often bewildering—task. This article outlines an easy process to facilitate reimbursement.
By Amy J. Aronsky, DO, FAASM
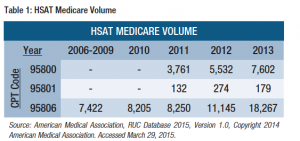
In 2013, the Centers for Medicare and Medicaid Services (CMS) reported Medicare utilization of home sleep apnea testing (HSAT) to be approximately 18,000, compared to 11,000 in 2012, and these numbers are continuing to rise (see Table 1).1
Utilization by commercial payors has grown more significantly, although regional variation exists. Commercial payors are increasingly requiring HSAT as a first-line diagnostic test for adult patients with a high pretest probability of obstructive sleep apnea (OSA) in the absence of comorbid medical conditions or suspected concomitant sleep disorders, which could limit the predictive value of at-home testing.
HSAT allows patients to be diagnosed with OSA from data obtained outside of the sleep laboratory. And HSAT costs less than in-lab polysomnography. Today, the national average Medicare global payment for HSAT (95806) is $169 compared to $625 for in-lab attended polysomnography (95810).1
To help ensure accurate coding and to facilitate HSAT reimbursement, consider these four steps.
Step 1: Determine the Type of HSAT Device Used
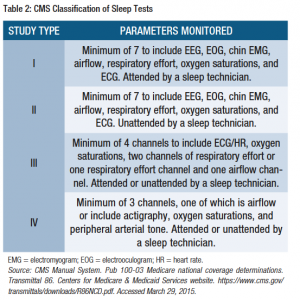
The classification used by CMS differs from the original description of portable monitoring in Standards of Practice: Portable Recording for the Assessment of Obstructive Sleep Apnea in 19942 and the more recent description by Collop et al.3 Type I studies are those sleep studies performed in the sleep laboratory and attended by a sleep technician. Type II sleep studies are performed unattended by a sleep technician. Type III and IV sleep studies may be performed attended or unattended by a sleep technician.
Physiologic parameters monitored are used to classify the type of HSAT device (see Table 2).4
Step 2: Apply the CPT and/or HCPCS Code
Sleep testing procedures are described by Current Procedural Terminology (CPT) codes, which are copyrighted and maintained by the American Medical Association. These CPT codes are found in the series between 95800 and 95811; 95782, 95783. The HSAT codes are 95800, 95801, and 95806. Use of the appropriate CPT code is determined upon the physiologic parameters monitored (see Table 3).
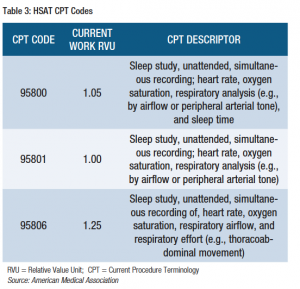
However, the previously described CMS HSAT classification of type III and IV sleep tests differs from CPT classification parameters. The HSAT study type may not exactly correlate with the CPT code.
To clarify, for a patient who has an unattended home sleep study meeting the requirements of a type III test, use code 95806:
“95806 Sleep study, unattended, simultaneous recording of, heart rate, oxygen saturation, respiratory airflow, and respiratory effort (e.g., thoracoabdominal movement).”
For a patient who has an unattended home sleep study using three or more parameters but not meeting the criteria for 95806, either 95800 or 95801 is used.5
Reporting 95800 includes a measurement of sleep time and 95806 describes a measurement of respiratory airflow and effort.
For accurate coding, 95800, 95801, and 95806 must include 6 hours of recording time. If less than 6 hours of recording data is obtained, modifier 52 should be appended to the HSAT code to indicate a reduced service and subsequently reduced reimbursement. If a physician codes for HSAT interpretation only, modifier 26 should be appended to specify the professional component of the service. When only the technical component of the procedure is coded, modifier TC is applied.
In 2008, CMS created G-codes (G0398, G0399, and G0400) to describe HSAT services. The G-codes were published prior to the establishment of the CPT codes. The G-codes are found in the Healthcare Common Procedure Coding System (HCPCS) Level II codebook and are maintained and valued by CMS.
G-codes are procedure codes developed by CMS to identify products, supplies, and services not included in the CPT codes for which there is a programmatic operating need to separately identify them on a national level.6 Reimbursement is determined regionally by the specific Local Coverage Determination (LCD).
“G0398: Home sleep study test (HST) with type II portable monitor, unattended; minimum of 7 channels: EEG, EOG, EMG, ECG/heart rate, airflow, respiratory effort and oxygen saturation.
G0399: Home sleep test (HST) with type III portable monitor, unattended; minimum of 4 channels: 2 respiratory movement/airflow, 1 ECG/heart rate and 1 oxygen saturation.
G0400: Home sleep test (HST) with type IV portable monitor, unattended; minimum of 3 channels.”
Some Medicare contractors and commercial payors will mandate the use of G-codes and will not accept CPT codes when reporting HSAT. Be certain to understand the carrier’s requirement when submitting the claim. Typically, the code that best describes the procedure should be reported. However, when services are similar, reporting the CPT code is preferentially accepted.7
Step 3: Know the HSAT Coverage Guidelines for Each Health Insurance Payor
Each health insurance payor has published coverage guidelines available on its website. Commercial payor guidelines are developed based upon accepted best practices and may differ from CMS National Coverage Determination (NCD). It is also important to access the specific CMS Local Coverage Determination. The LCD provides additional regulations for each CMS coverage region, and HSAT coverage and reimbursement often varies between jurisdictions. Review of coverage guidelines will outline topics such as: indications for sleep testing, types of HSAT devices approved for use, and number of nights of HSAT testing permitted per billing procedure (typically 1 night). Specific insurance carrier policies also should be evaluated to address other reimbursement questions. Are sleep facility and/or HSAT accreditation required for reimbursement? Must the interpreting HSAT physician be board certified in sleep medicine? Familiarization with payor coverage guidelines and policies is an important step in correct coding for HSAT.
Whenever possible, obtain prior authorization for HSAT testing from insurance payors. Prior authorization requirements are based upon the health plan’s clinical guidelines and allow the qualified healthcare professional the opportunity to justify the need for sleep testing. Obtaining authorization for sleep testing up front can minimize inconvenience for the patient and the provider later.
Step 4: Report the Corresponding ICD-9 Diagnosis Code(s)
While the CPT codes and G-codes describe the HSAT procedure, International Classification of Diseases (ICD)-9 diagnosis codes support the medical necessity for the procedure. ICD-9 codes accepted for HSAT testing are typically described in the payor’s clinical guidelines and are required for reimbursement. Include the appropriate ICD-9 code to codify the clinical indications for HSAT testing.
Despite the relative simplicity of HSAT, the correct coding may seem complex when compared to other sleep testing codes. Using the correct codes to report the HSAT services documented will facilitate reimbursement by health insurance payors.
Amy J. Aronsky, DO, FAASM, is medical director at CareCentrix and primary advisor to the AMA’s Relative Value Scale Update Committee (RUC). She is a member of Sleep Review’s editorial advisory board. The author thanks Marc Raphaelson, MD, for editorial assistance.
References
1. American Medical Association, RUC Database 2015, Version 1.0, Copyright 2014 American Medical Association. Accessed March 29, 2015.
2. Thorpy M, Chesson A, Ferber R, et al. Practice parameters for the use of portable recording in the assessment of obstructive sleep apnea. Sleep. 1994;17(4):378-392.
3. Collop NA, Tracy SL, Kapur V, et al. Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clin Sleep Med. 2011;7(5):531-548.
4. CMS Manual System. Pub 100-03 Medicare national coverage determinations. Transmittal 86. Centers for Medicare and Medicaid Services website. https://www.cms.gov/transmittals/downloads/R86NCD.pdf. Accessed March 29, 2015.
5. Nelson M. Coding and billing for home (out-of-center) sleep testing. Chest. 2013;143(2):539-543.
6. American Gastroenterological Association, Coding FAQs – CMS 2015 G-codes for lower endoscopy procedures, http://www.gastro.org/practice/coding/coding-faqs-cms-2015-gcodes-for-lower-gi-endoscopy-procedures. Accessed March 28, 2015.
7. HCPCS decision tree. Centers for Medicare and Medicaid Services website. http://www.cms.gov/MedHCPCSGenInfo/Downloads/HCPCS_Decision_Tree_and_Definitions.pdf. Accessed March 29, 2015.



