How to get your whole team on board with dental sleep medicine.
The prevalence and under-treatment of obstructive sleep apnea (OSA) in the general population is alarming. To begin, an estimated 30 million Americans have the disorder, yet 80% of those cases remain undiagnosed.1 Couple that with the fact that the population of Americans age 65 and older—a group at high risk for OSA—is projected to more than double from 46 million to over 98 million by the year 2060.2
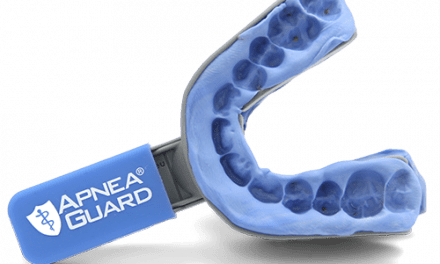
For those who have been diagnosed with OSA, continuous positive airway pressure (CPAP) is the accepted gold standard for treating the condition. However, low adherence rates mean many patients remain ineffectively treated, leaving them at risk for a host of associated comorbidities and in need of an alternative option. The convergence of these realities provides dentists a golden opportunity to help address this public health epidemic by incorporating dental sleep medicine (DSM) and the administration of oral appliance therapy (OAT) into their dental practices.
When implemented correctly and strategically, DSM can be exciting and rewarding—financially and otherwise. In addition to providing a profit center, DSM has the potential to save lives and save relationships. For me personally, the reward comes in the form of patients who are happy to see me when I walk into an appointment. As dentists know, that’s frequently not the case when walking into a dental operatory.
In this article, I will offer advice about how to get the whole team on board so that DSM is a bona fide profit center—not just a hobby.
Staffing a DSM Practice
It doesn’t take many team members to get sleep going in a dental practice. The key roles in any successful DSM practice are going to be: the dentist, a sleep assistant, a patient coordinator, and a medical insurance coordinator. For practices just starting out, one person may even be able to take on two or three of the roles, until patient load requires further separation of responsibilities.

Sleep Dallas sleep assistant, April Fields, demonstrates to a patient how to adjust her appliance. Photo courtesy of Sleep Dallas.
Sleep Assistant: The sleep assistant is to the dentist what a physician assistant is to an MD. Their primary responsibility is patient care, and they assist the dentist in all aspects of the treatment process. From pre-screening and scans/impressions to appliance fitting and adjustment, sleep assistants should be able to execute treatment administration, with the doctor providing oversight for protocol adherence and patient treatment outcomes. Some of these duties might not be allowed in your state, so adherence to the regulations is important.
Because the sleep assistant spends the most time with the patient, selection for this role should not be taken lightly. For dentists with existing staff to choose from, a dental hygienist or assistant who loves people and has a keen ability to gain the respect and trust of a patient is a prime candidate. However, if filling the role requires an outside hire, it’s not necessary for sleep assistants to have dental training. Medical assistants, for example, are a great option. Focus on hiring a person with the right personality and get them training for the rest.

Sleep Dallas patient coordinator greets a sleep patient arriving for his appointment. Photo courtesy of Sleep Dallas.
Patient Coordinator: This is the simplest role to transition or absorb with existing administrative staff. The key is to ensure that whoever is going to be scheduling sleep appointments is properly trained and armed with the knowledge necessary to speak confidently on the subjects of sleep apnea, OAT, and billing related topics.
Medical Insurance Coordinator: For dentists accustomed to working with dental insurance, the learning curve associated with medical insurance claims can be steep and frustrating. It’s not an impossible feat, but there will need to be a person dedicated to the task and willing to undergo the necessary training. For new practices, the patient coordinator or the sleep assistant may be able to take on the challenge. Once the patient load hits critical mass, however, this is a position that will require a dedicated staff member or contracting with an external third-party billing company.
Dentist: Sure, this is an obvious one, but I think it’s worth mentioning nonetheless. Remember when I mentioned the physician assistant and MD analogy a bit ago?
The doctor’s most important role is to ensure all team members are properly trained and to oversee systems and protocols—to create a work environment in which team members can execute efficiently and effectively. Once that’s been accomplished, the sleep practice will run like a well-oiled machine, allowing the doctor to continue serving dental patients or take on other specialties to help grow the practice.
Proper Training Is Key to Success
Just as we’d expect every team member in a dental practice to be able to speak knowledgeably and confidently about any number of dental procedures or related topics, so must we prepare the sleep staff to be able to speak to sleep, snoring, OSA, and OAT. As with nearly any endeavor, preparation is key, and that means everyone in the practice—from the administrative staff to the sleep assistants—should be properly trained.
For doctors, the actual amount of required DSM education varies by state. In Texas, for example, dentists are required to complete 12 hours before they can administer OAT. For each subsequent year, the dentist must complete three hours of continuing education (CE).3
In my experience and what I tell dentists who ask my advice, 30 hours of CE annually (for both the doctor and staff) is a great goal. I recommend completing as much as possible—after all, you can never learn enough. I even recommend taking a few courses on the same topic from different instructors, as each is going to provide a unique perspective.
When searching for quality education about sleep and DSM, it’s best to stick with recognized national organizations such as the American Board of Dental Sleep Medicine (ABDSM), American Sleep and Breathing Academy (ASBA), American Academy of Dental Sleep Medicine (AADSM), and Academy of Clinical Sleep Disorders Disciplines (ACSDD).
In addition to the accreditations these organizations provide for the doctor and practice, they are also an excellent resource to find recommendations and options for CE.
Another thing I recommend highly is to shadow well-established DSM practices. A day spent cross-training at a successful practice can often be more impactful than attending a conference because it gives the doctor and the other team members the chance to observe the entire process and learn efficiencies they can bring back to their own practice.
Make Sure Everyone Is on the Sleep Bus
Just as with any business, building a successful sleep practice takes time, patience, and dedication. For dentists adding the discipline to their existing dental practices, one of the main challenges they’ll face is gaining buy-in from team members who may be comfortably executing their dental-focused roles but less enthusiastic about taking on a new challenge.
Once the doctor has made the leap—and I mean two feet in because “dabbling” isn’t likely to yield success—the first step is to identify the change agents within the existing team. Enlist those who are hungry and willing to learn something new. Like I said earlier, there doesn’t need to be a lot of team dedicated to sleep to start off, but those who are play a significant role in the success and profitability of the practice.
One tactic I have found to drive change and buy-in is to provide treatment to a family member or friend of a team member. Does Sherry’s husband snore? Is Dave’s brother always tired? Does Joan’s husband refuse to wear his CPAP? It’s hard to deny the value and life-changing impact of an oral appliance if a loved one reports feeling happier, healthier, and more refreshed after treatment.
Secondly, dedicate physical space, time, and effort to the sleep practice. Make the office look like sleep is important by posting information about snoring, sleep apnea, and OAT in the waiting rooms and throughout the practice. Launch earnest marketing efforts to drive patient appointments.
And most importantly, get training for every team member who will be dedicated—in full or in part—to the sleep practice.
Kent Smith, DDS, DABDSM, ASBA, is the founding director of Sleep Dallas, a dental sleep medicine practice serving the Dallas-Fort Worth metroplex. Smith is president of the American Sleep and Breathing Academy, a Diplomate of the American Board of Dental Sleep Medicine, and is on the advisory committee of the Australasian Academy of Dental Sleep Medicine. In addition to running his practice, Smith is the founder and primary facilitator of 21st Century Sleep Seminars, a series of training events that prepares dental professionals to incorporate dental sleep medicine into their practices. Smith has also created curriculum for a course focused on recognizing and treating sleep breathing disorders at the Las Vegas Institute of Advanced Clinical Studies.
TOP PHOTO: Kent Smith, DDS, of Sleep Dallas explains to a patient how oral appliance therapy addresses his condition. Photo courtesy of Sleep Dallas.
References
1. Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013 May 1;177(9):1006-14.
2. Mather M, Jacobsen LA, Pollard KM. Aging in the United States. Population Bulletin. 2015 Dec;70(2):3.
3. Rule § 108.12: Dental Treatment of Obstructive Sleep Apnea.” Texas Administrative Code. https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=T&app=9&p_dir=N&p_rloc=121953&p_tloc=&p_ploc=1&pg=3&p_tac=&ti=22&pt=5&ch=108&rl=12





Very nice and interesting description about Dentistry in Sleep Disorders, I do have some Qs for you: ” with DAT, how will be able to treat Central Sleep Apnea, Central Sleep Hipopneas, Alpha intrusion Sleep, Alpha Delta Sleep, RBD ( Rem Behavior Disorders, PLM, PLMD and many others disorders, when with CPAP, BIPAP, ASV and AVAP. I spent more than 25 yrs in Sleep Med and I did Disensitization on many noncompliant patients, what I,m missing, I think I need to be more informed about DATs…..Thank you very much for your willingness to answer my Qs, I can even provide you with some information about Sleep…..Txs again….JT….PS.will be very nice to be able to talk with somebody who knows Sleep ( maybe I can learn more..)..Goodluck to all of you, Great Succes…JT…