More than 60 different OAs are on the market, with notable design variations. A dentist provides insights on six general categories—mono-block, hinge-based, compression-based, traction-based, other, and trial/temporary—to assist in selecting the correct device for a given patient.
Sleep-disordered breathing (SDB) spans a continuum from snoring to upper airway resistance syndrome to obstructive sleep apnea–hypopnea syndrome (OSAHS). The availability of oral appliances (OAs) allows for an alternative therapy for patients with obstructive sleep apnea (OSA). Oral appliances mechanically increase the pharyngeal space by advancing the mandible and/or the tongue. More than 60 different oral appliances are in use, with considerable variations in design.
Types of Oral Appliances
Oral appliances for the management of OSA are of different constructional design and made of various dental materials used in clinical situations.1 The different OA designs may influence therapeutic outcome, compliance, and persistence of usage.
Several papers have compared two types of OA that differ in their ability to open the mouth during sleep in the protrusive position, and in the splint material, regarding their subjective and objective short- and long-term treatment efficacy.2-5 The general conclusion in these papers was both oral appliances improved SDB and symptoms, and both are valid therapeutic options for selected patients with OSA. The only difference in the studies was the patient’s preference of device based on comfort.
Dentists’ Opinions
When speaking to dental colleagues on their favorite devices for the management of OSA, a wide range of appliances were mentioned based on the clinician’s favored device. Some clinicians suggest that limiting the number of different appliances helps to reduce confusion in the office. However, others speak of offering a variety of appliances so the appropriate device can be matched to the patient.
Appliances that are available with a soft liner are preferred by some due to ease of fit and speed of delivery; they are gentler on the teeth, particularly helpful when dealing with heavily restored teeth, veneers, or crown and bridge. In my opinion, it is important to become familiar with the different appliance styles available in order to best match the device to various patient presentations and insurance requirements.
Some clinicians I have polled typically select two or three appliances that are suitable for their patient. In doing so, they allow their patient to pick the appliance that most appeals to them. The rationale being that if a patient selects the appliance, the adherence may be higher. In contrast, many clinicians feel very strongly that appliance choice is the dentist’s decision, based on all the clinical findings for that case. I favor the latter method because providing several options for devices may require you to be in the treatment room for longer periods of time discussing the pros and cons with the patient on the various choices between appliances, and the patient still depends on your input.
Roles of Oral Appliances
If we look at the fundamental role of oral appliances for management of OSA, they function like a jaw thrust maneuver for opening one’s airway—ultimately preventing the mandible from falling back during sleep. As a result of posturing the mandible forward, they also provide a lateral improvement of the velopharynx, which is similar to what a CPAP does.5-8
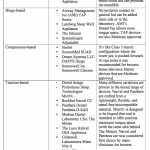
Due to the number of OAs available in the market, we will summarize them into six general categories to display their similarities.
Table 1. OralApplianceCategories
In the following table are guidelines of frequently encountered clinical situations and a suggested recommendation of OA choices.
Table 2. OralApplianceClinicalSituations
If OA is not adequately managing your patients’ OSA, then considerations of abandoning OA treatment may be an option. However, utilization of combination therapy may be appropriate in these clinical situations.9-11 Combination therapy of OA and nasal CPAP is effective in normalizing respiratory disturbances of sleep apnea.
In conclusion, I believe it is all about getting to know the appliances you are using, and all their nuances. This will allow you to best match them to your patient and deal with issues that may arise due to their use.
Mayoor Patel, DDS, MS, is the owner of Atlanta’s Craniofacial Pain and Dental Sleep Center of Georgia.
References
1. Hoffstein V. Review of oral appliances for treatment of sleep-disordered breathing. Sleep and Breathing. 2007;11(1):1-22.
2. Ghazal A, et al. A randomized prospective long-term study of two oral appliances for sleep apnoea treatment. Journal of Sleep Research. 2009;18(3):321-8.
3. Bloch KE, et al. A randomized, controlled crossover trial of two oral appliances for sleep apnea treatment. American Journal of Respiratory and Critical Care Medicine. 2000;162:246-51.
4. Lawton H, Battagel J, Kotecha B. A comparison of the Twin Block and Herbst mandibular advancement splints in the treatment of patients with obstructive sleep apnoea: a prospective study. European Journal of Orthodontics. 2005;27(1):82.
5. Sutherland K, et al. Comparative effects of two oral appliances on upper airway structure in obstructive sleep apnea. Sleep. 2011;34(4):469-77.
6. Chan ASL, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010;65(8):726-32.
7. Ryan C, et al. Mandibular advancement oral appliance therapy for obstructive sleep apnoea: effect on awake calibre of the velopharynx. Thorax. 1999;54(11): 972-7.
8. Chan ASL, et al. Nasopharyngoscopic evaluation of oral appliance therapy for obstructive sleep apnoea. European Respiratory Journal. 2010;35(4):836-842.
9. El-Solh AA, et al. Combined oral appliance and positive airway pressure therapy for obstructive sleep apnea: a pilot study. Sleep and Breathing. 2011;15(2):203-8.
10. Upadhyay R, et al. Management of severe obstructive sleep apnea using mandibular advancement devices with auto continuous positive airway pressures. Lung India. 2015;32(2):158-61.
11. de Vries GE, et al. Continuous positive airway pressure and oral appliance hybrid therapy in obstructive sleep apnea: patient comfort, compliance, and preference: a pilot study. Journal of Dental Sleep Medicine. 2016;3(1):5-10.








The charts are so biased – the contributor is clearly only a Narval, Panthera and TAP user.