An expert practitioner who has treated hundreds of shift workers describes a realistic, sustainable way for sleep health professionals to help this patient population.
Our society couldn’t function without shift workers. Imagine life without overnight transportation, public safety, 24-hour healthcare, or national security. Indeed, roughly one in five working Americans works some sort of nontraditional shift. Unfortunately, shift work takes its toll. Shift workers experience more health problems, including metabolic syndromes, cardiovascular disease, cancer, gastrointestinal problems, and depression, as well as worsened quality of life.
Although the only cure for shift work is to stop working shifts, every sleep health professional evaluates patients with shift work disorder. More important, most patients benefit greatly from treatment. But treatment can be challenging, especially when it comes to sleep-wake scheduling. For example, even after treating hundreds of shift workers from a dozen professions, I’ve never met one who maintained a consistent sleep-wake schedule, 7 days per week. Patients need a more realistic approach.
Anchoring sleep is among the most powerful recommendations for shift workers on many schedules because it can increase quantity of sleep and make the timing of sleep more consistent, without unduly sacrificing quality of life on non-workdays. Although anchoring sleep can be easier said than done, when implemented properly, it is realistic and sustainable, and it produces great results. In this article, you’ll learn my simple yet powerful system for sleep anchoring.
What Is Sleep Anchoring?
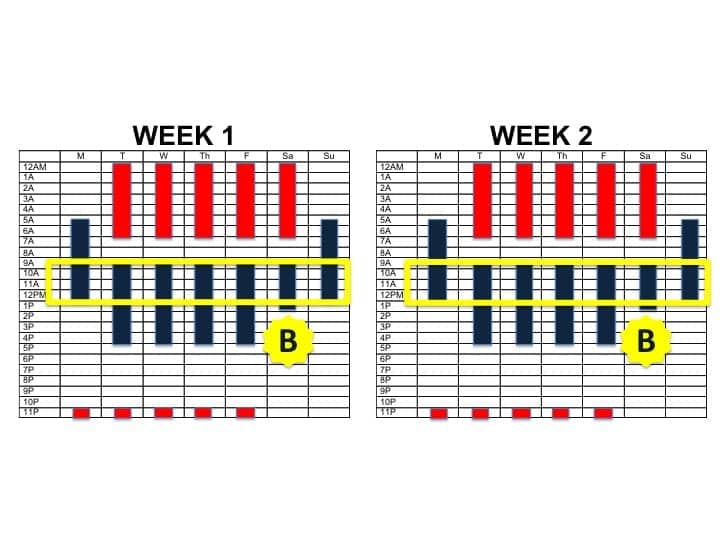
Like the anchor that keeps the boat steady and secure, anchor sleep provides a guidepost for the body clock. As depicted in the above figure, an anchored sleep schedule is one where several hours of sleep will always overlap, every night, regardless of whether it is a workday. This anchor point maintains consistency even when schedules change.
How to Anchor Sleep
The single most powerful way to help your patients anchor their sleep is to create a proactive sleep schedule that will ensure the needed overlap from day to day. This is best accomplished using a visual shift work sleep diary, so that patients can fill in their work schedules ahead of time, then plan their sleep opportunities. The visual schedule becomes a powerful guide to enable patients to see the possible times when they can sleep—and heightens awareness of schedule conflicts, and how little sleep will be obtained without purposeful effort.
Steps to anchor sleep:
- Enter work schedule in shift work sleep diary.
- Designate 7 or more hours for sleep per 24-hour period.
- Designate 3 to 4 hours of “anchor sleep” that will remain constant on both workdays and non-workdays.
- Stick to the schedule.
Overcoming Barriers to Sleep Anchoring
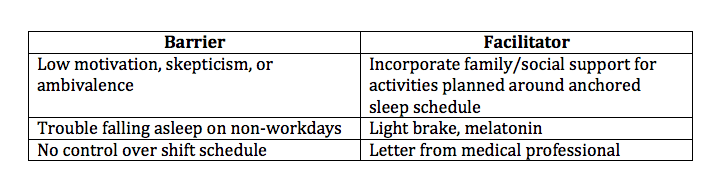
As with all things shift work, anchoring sleep is easier said than done. And there is no one “magic bullet” solution to working shifts. Good sleep hygiene, planned naps, post-shift wind-down routines, and, when indicated, wake-promoting medications should all be tools in your practitioner toolbox. That said, anchoring sleep is a very powerful and highly effective strategy for sleep-wake scheduling, so it’s important to know what to expect when you implement it.
The single biggest barrier to adherence is patient uncertainty or hesitation. For example, many patients want to follow “normal” schedules on their non-workdays to spend time with their families or to engage in recreational activities. As a result, anchoring sleep can sound unpleasant or outright impossible. Patients can perceive that an anchored sleep schedule will cause them to miss out on important experiences, worsening the shift work experience.
To maximize patient adherence, a motivational approach is essential. You must rapidly identify your patients’ real goal for treatment, and tailor your treatment plan (including sleep anchoring) to meet exactly these goals. (Read about increasing adherence in sleep medicine in my 2012 article “Cognitive Behavioral Treatment in Action.”)
The second most perceived barrier is a difficulty falling asleep earlier on non-workdays. Because it is nearly impossible to shorten the circadian phase, shift workers are often not yet sleepy at their prescribed anchor sleep time, especially on their first night off after consecutive workdays.
One solution to the difficulty falling asleep on transition days is to employ a “light brake.” First developed at the University of Chicago (eg, Smith, Fogg, & Eastman, 2009), this approach entails curtailing the sleep period on the last night of consecutive shifts, to increase sleep drive on the subsequent sleep period (see sidebar “Barriers and Facilitators for Sleep Anchoring”). Similarly, the American Academy of Sleep Medicine recommends 3 mg melatonin prior to daytime sleep for night shift workers (Morgenthaler et al, 2009), which can also be very helpful.
Family Support for Sleep Anchoring
When shift workers are married, shift work is a family affair. Indeed, wanting to provide for one’s family is often the primary reason many shift workers work shifts in the first place! So whenever possible, include a spouse or significant other in the care plan. In my clinical and training experience, nearly every spouse will be supportive of a plan that helps the shift worker, and in turn the family, once they understand the problems and strategic approach.
Encourage your patient to invite a loved one into a treatment encounter. If this is not possible, encourage your patient to discuss solutions and problem-solve at home to overcome barriers in anchoring sleep. This might entail reassigning household chores, planning family activities on weekend afternoons instead of weekend mornings, or simply maintaining a quiet household during mom’s or dad’s sleeping hours.
Improve Sleep Anchoring with the Wickwire Funnel Framework
To give you a sense of how to quickly, clearly, and effectively explain sleep anchoring to patients, here is a sample dialogue using my powerful framing system, the “Wickwire Funnel Framework” (WFF). (Read more about the WFF in my January 2016 article “How to Talk to Insomnia Patients—Faster, More Effectively, and With Less Frustration.”) Following this approach will help you take better care of your shift work patients faster and with less frustration than ever before.
You: The problem is that your sleep yo-yos back and forth between workdays and non-workdays, so your body clock is all over the place. The solution is to anchor your sleep by placing guiderails around your body’s sleep schedule. Make sense?
Patient: Yes, I’m with you.
You: Let me share two guiding principles to explain how this works. First, we are going to establish a consistent, regular sleep-wake schedule for workdays and another for non-workdays. Second, we are going to anchor your sleep and make sure that there is overlap of at least 2 to 4 hours every single day. This will help keep your body clock on track. Does that make sense?
Patient: Yes. But how the heck do we do that?
You: Good question—it’s easier than you think. The first step is to enter your work schedule in this shift work sleep diary. Next, plan out 7 or more hours for sleep per 24-hour period, with one consistent schedule for workdays and another for non-workdays. Finally, make sure that 3 to 4 hours of sleep are anchored and overlapping on both workdays and non-workdays. Like this [demonstrate]. Do you follow?
Patient: Yes, but I never feel sleepy that early on my off days.
You: That’s a very common concern, and I have a few ideas. Let’s discuss which makes the most sense for you…
Summary

Many of our nation’s most noble professions require working nontraditional shifts. Unfortunately, shift work is often at odds with evolution as humans are diurnal creatures. As a result, shift workers are at increased risk for multiple medical problems and worsened quality of life related to not getting enough sleep, suffering poor quality sleep, and experiencing irregular timing of sleep. Sleep anchoring is a powerful way to help patients adapt to their work schedules while maintaining quality of life. Follow the steps in this article and leverage this powerful system to help your shift working patients get the rest they need and the sleep they deserve.
Emerson M. Wickwire, PhD, is assistant professor at the University of Maryland School of Medicine and director of the insomnia program at the University of Maryland Medical Center. He is the author of over two dozen scientific articles and several patient guides including the Shift Work Survival Guide, which will be available on Amazon. He is associate editor of the Journal of Clinical Sleep Medicine and a proud member of Sleep Review’s editorial advisory board.





