As automatic PAP device usage grows, it’s imperative you’re able to separate fact from fiction.
“The great enemy of the truth is very often not the lie, deliberate, contrived, and dishonest, but the myth, persistent, persuasive, and unrealistic.”
President John Kennedy probably did not have automatic (also known as auto-titration) positive airway pressure (APAP) devices in mind when he made the above statement at a Yale University event. But the quote’s wisdom, as it applies to unrealistic expectations for sleep apnea treatment machines, certainly rings true in sleep medicine today.
Understanding the difference between myth and reality is essential for healthcare professionals to treat patients appropriately.
“In order to optimize the efficacy of APAP, clinicians and sleep technologists who use it to manage patients with obstructive sleep apnea (OSA) should understand its unique algorithms for identifying and responding to respiratory events, and for reporting and addressing mask leaks,” says Teofilo Lee-Chiong, MD, chief medical liaison for Philips Respironics. “They should familiarize themselves with the different ways to troubleshoot problems that may arise, as well as measures that can enhance patient comfort when using APAP.”
In line with that sentiment, here is our effort to dispel seven common misconceptions about APAP technology and its use.
Myth 1: APAPs are “experimental”
Automatic CPAP (one of several common names for APAP) has been extensively researched over the past 20 years, according to Steven Coughlin, director of Strategy, Health Economics and Reimbursement with Philips. Several national and international medical societies, such as the American Academy of Sleep Medicine (AASM), recommend APAP for the treatment of OSA based on the strength of clinical evidence. “A recent analysis of multiple international studies that utilized a variety of manufacturers’ devices concluded that APAP devices, when compared to CPAP, provide equivalent control of the AHI at a lower mean pressure, improving sleep stage distribution and providing comparable improvements in daytime sleepiness. Furthermore, patients showed a clear preference toward APAP devices and demonstrated marginally improved compliance when using this technology,” Coughlin says.
Jeremy Malecha, ResMed’s director of healthcare informatics, says ResMed’s first APAPAutoSet device was built in 1995 and has been clinically validated in numerous third-party tests and peer-reviewed journals for more than a decade.
Myth 2: APAPs aren’t for long-term use
APAPs are certainly intended to be long-term solutions, Malecha says. Contrasting with CPAP, APAP is designed to adjust with patients as their condition and physiology fluctuate. For example, ResMed’s newest S9 AutoSet automatically adjusts breath by breath, even as patients’ needs change—hourly, nightly, and from season to season to deliver the minimum pressure required for effective therapy.
Brian Palmer, director of marketing-sleep at DeVilbiss Healthcare, concurs that APAPs are ideal for long-term use. “Patients’ needs change over short and long periods of time. In a given night, a patient may have REM or positional induced apnea and need higher pressures only for short periods of the night. Over longer periods, a patient’s physiology or weight could change and therefore impact pressure requirements,” Palmer says.
Myth 3: APAPs wait for a breathing event before adjusting
APAP adjusts proactively verses reactively, Malecha says. ResMed’s AutoSet devices, for instance, have three lines of defense in identifying flow limitation early and preventing collapse of the upper airway. After patients fall asleep and their pressure needs begin to vary, AutoSet responds to three separate parameters, based on the degree of airway blockage: inspiratory flow limitation, snore, and apnea.
In DeVilbiss’ algorithm, snoring, which occurs before apneas and hypopneas, affects pressure change, which allows the unit to be proactive before apneas and hypopneas occur.
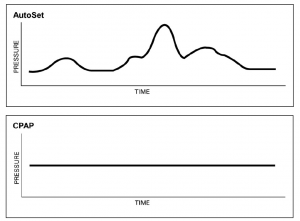
APAP pressure changes based on a patient’s needs at a specific time. CPAP pressure is maintained at a constant, generally based on a patient’s in-lab titration.
Myth 4: APAP is a set-it and forget-it system
Rachel Vicars, senior clinical research scientist at Fisher & Paykel, says both CPAP and APAP are not set-and-forget. Both require follow-up with patients to address issues like mask fit, compliance, and humidity. Some clinicians restrict the minimum and maximum pressure ranges to something they feel comfortable with, but this comes down to clinician experience.
Myth 5: All APAPs are the same
Each individual manufacturer has its own proprietary APAP algorithm, and each performs at a different level, responding differently to different breathing patterns, Malecha says.
Vicars says, “They are based on slightly different technology and respond to events differently. It is important you are using a manufacturer that has clinically validated its algorithms to ensure adequate treatment. These validations should be available for review. An important distinction between algorithms is the way they use events to ensure a timely response to sleep-disordered breathing events. For example, flow limitation is a precursor to other more severe sleep-disordered breathing events. An AutoCPAP needs to be able to respond to these flow-limited events in a timely manner to ensure that the more severe sleep-disordered breathing events (apnea and hypopnea) are minimized.”
Malecha adds, “In addition to differing APAP algorithms from manufacturer to manufacturer, there is now differentiation between APAP solutions for patients with OSA versus central sleep apnea. It is crucial for clinicians to understand the variability of products so they can select a product they feel is most appropriate for their patient.”
Myth 6: All AHIs are the same
According to Vicars, all machines report AHI, but not all machines are measuring the same thing. “How you define apnea and hypopnea greatly affects the AHI ‘number’ that you will see. The AASM defines an apnea as a reduction in flow of ?90% for ?10 s,1-2 but the definition for hypopnea is different depending on the year the standard was published, and whether you are using the recommended or alternative scoring methods. In all cases, the definition of hypopnea has both a flow component (ie, a reduction in flow of 30-90% for ?10 s)2 AND an oxygen desaturation or arousal component (ie, ?3% oxygen desaturation or associated with an arousal2). CPAP machines only use one measure to calculate the AHI—the airflow. They do not have the additional measures to calculate oxygen desaturation, or arousal as defined by AASM.
“Therefore, no CPAP machine can give you the same AHI as a PSG. Instead you are getting the manufacturer’s version of the AHI. No definition is more ‘correct’ than another—what is important is that the machine correlates with PSG-AHI (ie, a higher AHI indicates more events than a lower AHI) and that it is validated to treat.”
Myth 7: APAPs are good for everyone
Several studies have shown that AutoCPAP is equivalent to fixed pressure CPAP in treating OSA,3 Vicars says. “These studies are in a general OSA population, and therefore individual patient differences may not be taken into account. It is important to use caution when using AutoCPAP in certain populations, such as chronic heart failure, central sleep apnea, and obesity hypoventilation syndrome, as the algorithms may not have been validated to treat in these populations, and may not respond appropriately to the patient’s flow signal.”
So let’s put the last of those myths to bed.
Peter Blais, RPSGT, is a registered sleep technologist with the Center for Sleep Disorders at St. Mary’s Regional Health System in Auburn, Me. This is his first article for Sleep Review.
REFERENCES
1. Iber C, Ancoli-Israel S, Chesson A, Quan SF, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. 1st ed. Westchester, Ill: American Academy of Sleep Medicine; 2007.
2. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597-619.
3. Ip S, D’Ambrosio C, Patel K, et al. Auto-titrating versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: a systematic review with meta-analyses. Syst Rev. 2012;1:20.




